Clinical Trial Statistician - April Slee
Click for April's background info
Click for April's background info
April Slee: I am a post-graduate student at UCL department of primary care and population health. Infectious disease junkie. Clinical trial statistician. What I lack in knowledge I try to make up for in opinions (and will try to keep clear which is which). Current residence: Seattle, Washington.
Leave comments with messages of support
April's diary
Day 28
Don’t give up on remdesivir just yet
For the record, I was never jazzed about Gilead’s Ebola drug that has been repurposed to treat COVID-19. There is a glorious history of drugs that were meant to do 1 thing and ended up being really good at something else – sildenafil (Viagra) and minoxidil (Rogaine) are failed heart drugs and onabotulinumtoxinA (Botox) was supposed to treat crossed eyes. Remdesivir is one of those generic RNA antivirals that might help – as other antiviral drugs like oseltamivir (Tamiflu) might help, but the mechanism by which it would really shine in COVID-19 is murky to me.
The leaked data from Chicago that led to a huge jump in Gilead’s stock last week was inconclusive to me – it is great that the majority of the 125 patients were sorted out and discharged within a week, but there were a couple of deaths. And patients on mechanical ventilation or with liver and kidney problems were excluded.. Furthermore, my favorite complaint, there was no control group.
Among patients on “life-saving” ventilators, only about 1 in 10 survive. Remdesivir would have a place if it could prevent patients from getting to the point that they require ventilators, and there are some trials currently underway to find out if this drug could help the sickest patients. Based on a screenshot accidentally posted on WHO’s website, though, everybody seems ready to give up on this drug.
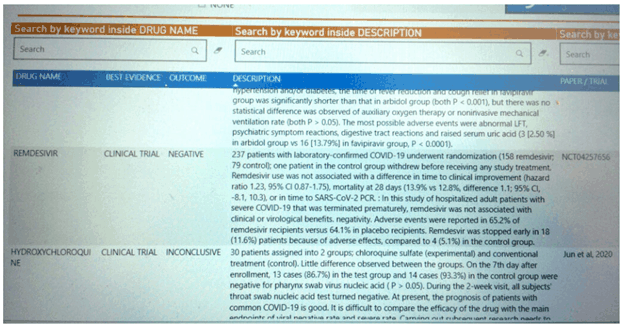
Here is what we actually know. There are 10 remdesivir studies listed on clinicaltrials.gov including the one that was leaked today.
I made a chart so we can follow along. I have bolded the ones that Gilead is actually paying for, which are ongoing. Note that 2 of them have a combined sample size of 7,600 patients. The data leaked today was the first trial, which had a planned sample size of 453 patients but only recruited 237 patients. The primary outcome is going the right way (you want the “risk” of clinical improvement to be > 1), but at half the planned sample size, it was not going to get a statistically reliable answer.
Usually when trials are stopped early for any reason other than overwhelming efficacy, it’s a very bad sign. But this trial was started at the tail end of the outbreak. The location is listed as Beijing, which didn’t have a lot of cases to begin with. One explanation for the early stop is that they literally ran out of COVID-19 patients to enroll. The study that started a week later in Wuhan has also been suspended, maybe for the same reason. Hopefully these studies didn’t get off to a late start because they got hung up for silly reasons in ethics committees, that virus seems to be going around too. Ethical oversight is essential but (thank God) COVID-19 may not wait.
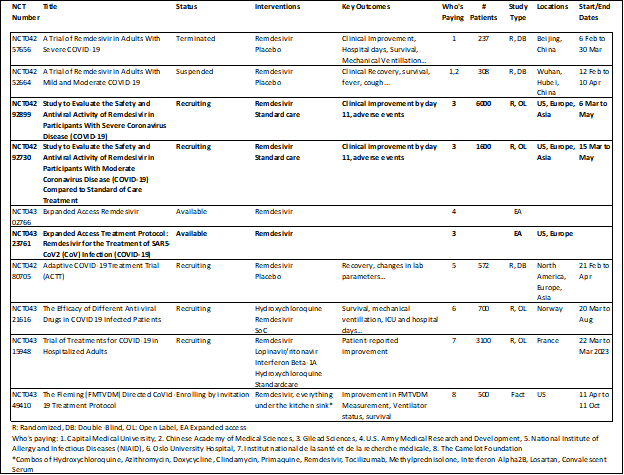
The big trials are due out next month, and I am going to wait for those before I draw any conclusions about this.
Day 25
Interview
Q: What has changed for you in the last week?
My partner has been sick, I have been in a fog of worry. Spent a lot of time watching him sleep, listening to him breathe. He is finally looking a little better today, so I am hopeful he is on the mend.
Q: What are you thinking about doing next?
Lately I’ve just been taking it one day at a time. Best I can do with this kind of uncertainty.
Q: Do you relish doing things that you never done before?
Not relish – I really hate being bad at things. But this pandemic has required me to do a lot of new things, learn a lot of new things, and I’ve just had to put my pride aside.
Q: Do you prefer to take on large or small projects?
I enjoy starting large projects, I’m better at finishing small ones.
Q: How do you feel when you see all the negativity about COVID19?
Interesting question. I think we coalesce around a crisis. Crisis makes us willing to make sacrifices for others. It gives us a common goal and makes our institutions and social fabric strong. And then we spend the next 80 years or so drifting apart, becoming a lot more individualistic and self-sufficient, before the next crisis pulls us back together.
My partner has been sick, I have been in a fog of worry. Spent a lot of time watching him sleep, listening to him breathe. He is finally looking a little better today, so I am hopeful he is on the mend.
Q: What are you thinking about doing next?
Lately I’ve just been taking it one day at a time. Best I can do with this kind of uncertainty.
Q: Do you relish doing things that you never done before?
Not relish – I really hate being bad at things. But this pandemic has required me to do a lot of new things, learn a lot of new things, and I’ve just had to put my pride aside.
Q: Do you prefer to take on large or small projects?
I enjoy starting large projects, I’m better at finishing small ones.
Q: How do you feel when you see all the negativity about COVID19?
Interesting question. I think we coalesce around a crisis. Crisis makes us willing to make sacrifices for others. It gives us a common goal and makes our institutions and social fabric strong. And then we spend the next 80 years or so drifting apart, becoming a lot more individualistic and self-sufficient, before the next crisis pulls us back together.
Everything about COVID-19 seems negative, but it is part of a pattern that maybe has always been. WWII was the last big crisis, for us the civil war prior to that. After each of these crises, there was a feeling of pulling together and pulling for each other that lasted for about 20 years, and then a period of rebellion when we try to figure out what kind of society we want to be since we are all in this together (the suffrage and civil rights movements came out of the last 2 of these periods). Then we just start drifting apart, doing what is best for us as individuals.
When it gets to the point that we are losing friends over political opinions, a crisis happens that brings us back together. And then the cycle starts over. So this is negative, yes, in the same way that winter is negative. And on the other side of it is a social climate that can’t be built any other way, if the past is any guide.
Q: How do you feel about being told to stay home?
I get that slowing the spread is the best we can do right now, and I believe reducing social contact is a good way to do that. But I get frustrated because I feel like we are doing our part by following the guidelines about social distancing and the government is not doing their part in getting wide-spread testing access in place, so it is starting to get frustrating.
Q: How do you feel about the Governments narrative on COVID19?
I think the real failures happened before the pandemic started. It is clear that we didn’t have a good plan to deal with something like this. Countries like South Korea and some countries Africa have dealt with infectious disease outbreaks more recently, and have had to learn some lessons from those.
Q: How do you feel about being told to stay home?
I get that slowing the spread is the best we can do right now, and I believe reducing social contact is a good way to do that. But I get frustrated because I feel like we are doing our part by following the guidelines about social distancing and the government is not doing their part in getting wide-spread testing access in place, so it is starting to get frustrating.
Q: How do you feel about the Governments narrative on COVID19?
I think the real failures happened before the pandemic started. It is clear that we didn’t have a good plan to deal with something like this. Countries like South Korea and some countries Africa have dealt with infectious disease outbreaks more recently, and have had to learn some lessons from those.
I just wish we had learned more from them. Hoping the government fails in response to this is like hoping that the pilot crashes a plane that we are all on. Whatever I think of our leaders personally, I am pulling for them to succeed in defeating this virus now.
Day 21
“…it was the spring of hope, it was the winter of despair…”
-Charles Dickens, A Tale of Two Cities
-Charles Dickens, A Tale of Two Cities
This entry is a total buzz kill. If you don’t have the emotional bandwidth for that, please stop here.
My latest hope has been that COVID-19 is a lot more infectious than we thought, and the proportion of patients who are asymptomatic is a lot higher than we thought. The initial calculations of R0 coming from Chinese scientists in Wuhan was around 2.5, meaning every infected person on average is infecting 2.5 new people and the doubling time for the total number of infected persons is about a week.
A recent estimate out of Los Alamos and published by the CDC re-estimates R0 to be around 5, which means the number of infected people would double every 3 days or so. . One antibody study of 1,000 people in Germany suggested an infection rate of about 15%, and a death rate for the same municipality of about 0.37%. The overall death rate in Germany (cases with 2 week lag / fatalities) is 4.76% as of 11 April. Taken together, this means we are sure missing a lot of cases, and so the fatality rates we are estimating (based on an underestimate of cases) are *way* too high. Great news! COVID-19 is not nearly as lethal as we thought.
Another recent study in Chicago screened people who were tested for COVID-19 for antibodies in addition to live virus. The results were that 10-20% were positive for COVID-19 but 30-50% were positive for antibodies, meaning that about twice as many patients had already survived the disease and now have some immunity compared to the number who currently have it.
You might be wondering why I’m not more excited about this news. If R0 is 5, that means in places with a substantial outbreak, many (most?) people have had COVID-19 and are producing antibodies against it. But there is an alarming report out of China showing that out of 175 recovered patients in Shanghai, 1 in 3 now have very low levels of antibodies or no antibodies at all . There is also this report out of South Korea raising the spectre of re-infections in recovered patients. I have been seeing reports of isolated cases like this for months, and I had hoped these were due to false negatives midway through the disease instead of actual re-infections. But the data that real re-infections happen is starting to pile up and I can’t explain it away anymore.
If countries like China and South Korea are finding 1 in 3 patients have no durable immunity and there are a substantial number of patients who have gotten COVID-19 twice, then SARS-COV-2 is more like the common colds which are also in this family of viruses in that the immunity is temporary (around 3 months). This property would make herd immunity extremely difficult to achieve, and it throws into question whether we will be able to make a vaccine for COVID-19. All vaccines “wear off”, but would it be worth mass distributing a vaccine if immunity only lasted 3 months?
Usually antibodies from having a disease (“natural immunity”) last longer than antibodies from a vaccine, so even 3 months might be a stretch. Maybe the COVID-19 vaccine could be like a flu shot but we would have to get it 4-6 times a year to maintain immunity. Super-lethal coronaviruses like SARS and MERS did seem to produce durable immunity though antibody levels dropped significantly after recovery. Stanley Perlman, a coronavirologist at the University of Iowa in Iowa City, has some data showing SARS antibodies 15 years after recovery. Whether those antibodies are strong enough to prevent a re-infection is unknown, but they should at least help.
A temporary vaccine would make containing isolated outbreaks easier using a technique called ring vaccination, where if someone gets COVID-19, we would vaccinate their contacts and their contact’s contacts. This technique helped us to wipe out Smallpox, but in that case, the vaccine will prevent disease if given several days after exposure. Whether a COVID-19 vaccine could have this property is unknown, but the incubation period (time from exposure to symptoms) is 7-17 days for Smallpox and 2-14 days for COVID-19, so the shorter incubation period may reduce the time for a vaccine wipe out already replicating virus.
So – maybe no immunity, and maybe no durable vaccine. Winter of despair. I feel about the same as I did at the end of The Empire Strikes Back.
Day 20
Guess I need a facemask…
Thanks to Dr. Amy Noland for this picture and permission to use it in my blog.
So – masks are good now. I made a couple last weekend. First, I had a look at this paper from researchers at Cambridge University comparing fabric masks to the kind we need to leave for our healthcare providers.They actually shot Bacillus atrophaeus bacteria (0.93-1.25 microns) and Bacteriophage MS virus (0.023 microns in size) at different household materials to see how what proportion of 1 micron particles they blocked. I have graphed their data compared to a reference standard surgical mask, which blocked 97% of particles. So the way to interpret this is a dish towel is 85.6% as effective as a surgical mask.
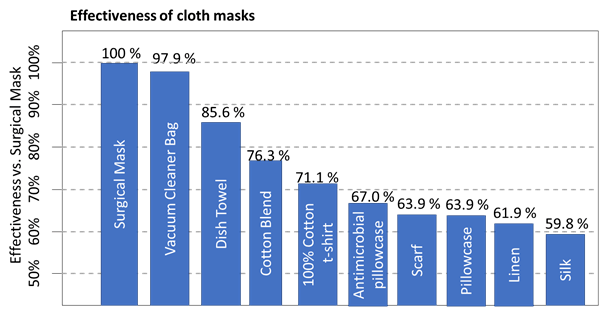
I wanted cloth masks that I could throw in the wash to avoid the kind of sterilization in Dr. Amy’s picture above, so I used 3 layers of fabric and skipped the vacuum cleaner bags. I used this pattern and with tight cotton on the outside, a layer of microfiber dish cloth and a layer of soft cotton. I used paper clips for the wire nose frame but wrapped them in a layer of duct tape so I wouldn’t get stabbed. Our surgeon general has a new-sew version demonstrated here.
This is my result:

Some people are putting HVAC filters in their masks and I really don’t advise this – they are often treated with chemicals that will do damage to your lungs that might be worse than what the virus will do. I made a couple cloth masks using the recipe above and put them in the washing machine as soon as I get home.
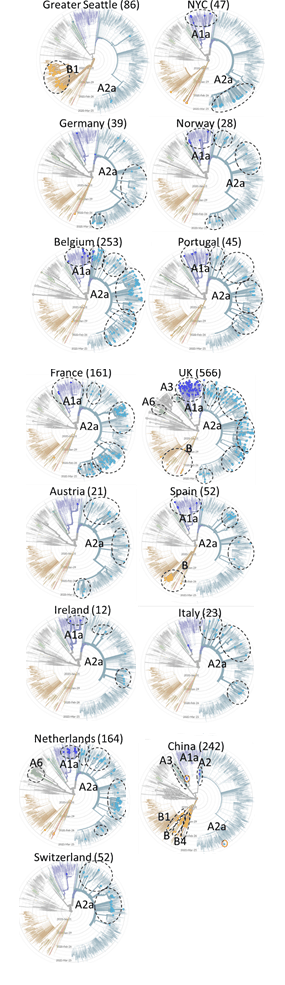
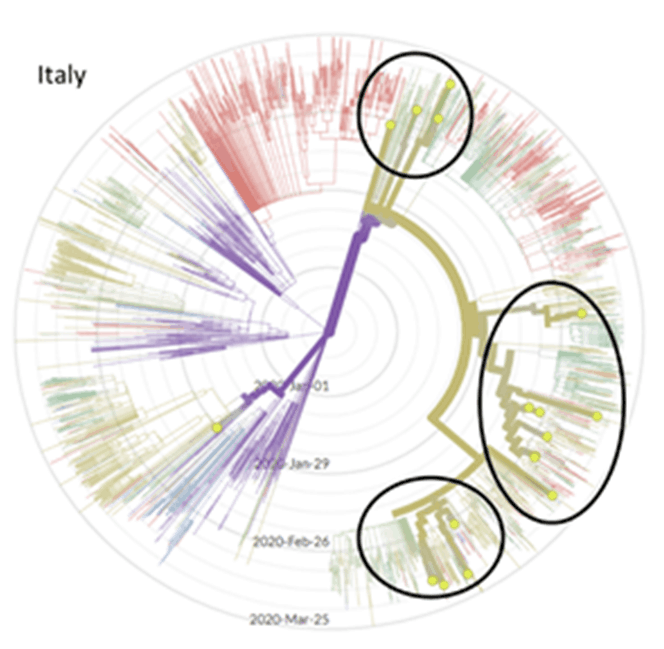
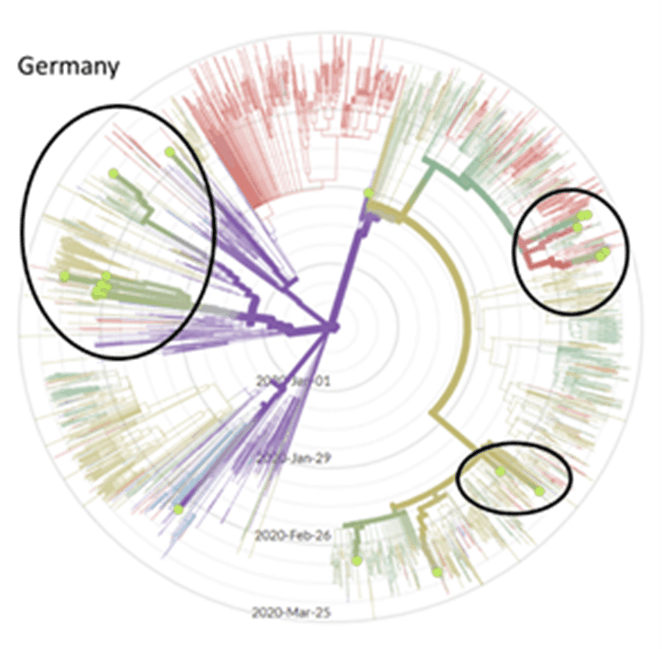
Day 19
Today I have more genomic evidence that Seattle is lucky, not good. A clade is a group of organisms believed to have evolved from a common ancestor. It comes from the Greek word klados, which means “branch”. Seattle and some of Northern California is infected with the B1 clade, while New York seems to be infected with A1a and A2a. Out of 242 samples from China, these clades are represented by only 1 sample each (though there are a few A2, which is the predecessor of A2a). I will need to look at this again when more data are available, especially from Italy.
Day 18
Most interesting question someone asked me today:
Why do all the estimates of the number of deaths show different things?
Yeah, 18,000 to 2,000,000 deaths in US does seem like quite a wide range. The fundamental formula for calculating who will die is simple:
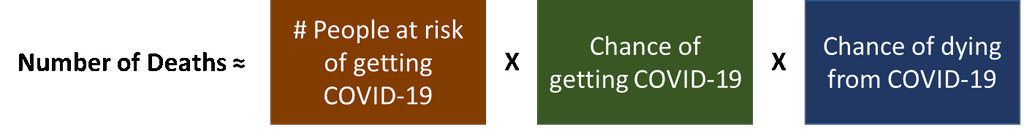
Since this is a novel coronavirus, we can simplify it further by assuming anyone can get it and no one has immunity because of previous exposure:

The first term number of people is a number we can look up for the US. It’s somewhere between 325 and 350 million (which is itself a wide range). But the second and 3rd term have several considerations:
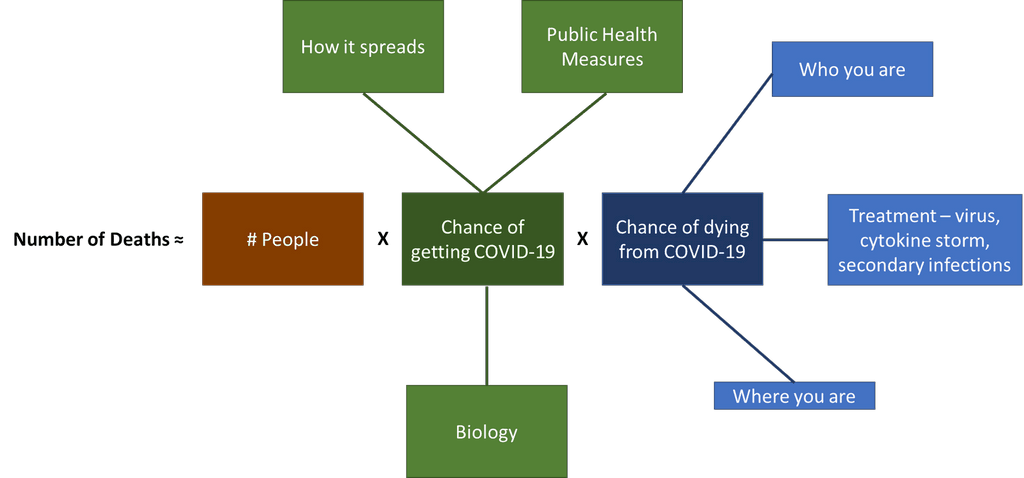
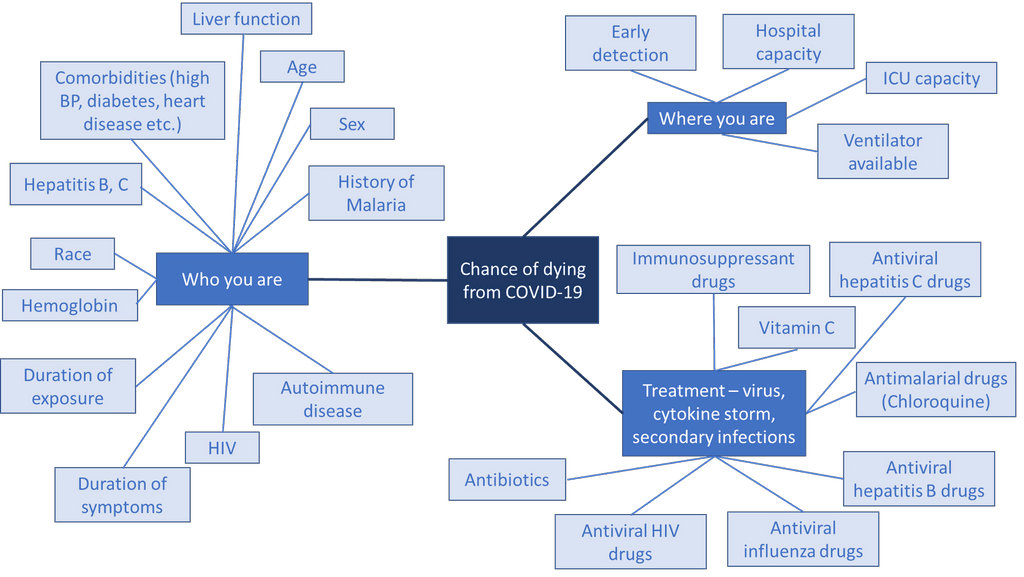
But there are known and unknown factors for each of these as well. For the chance of getting COVID-19, some considerations might be:
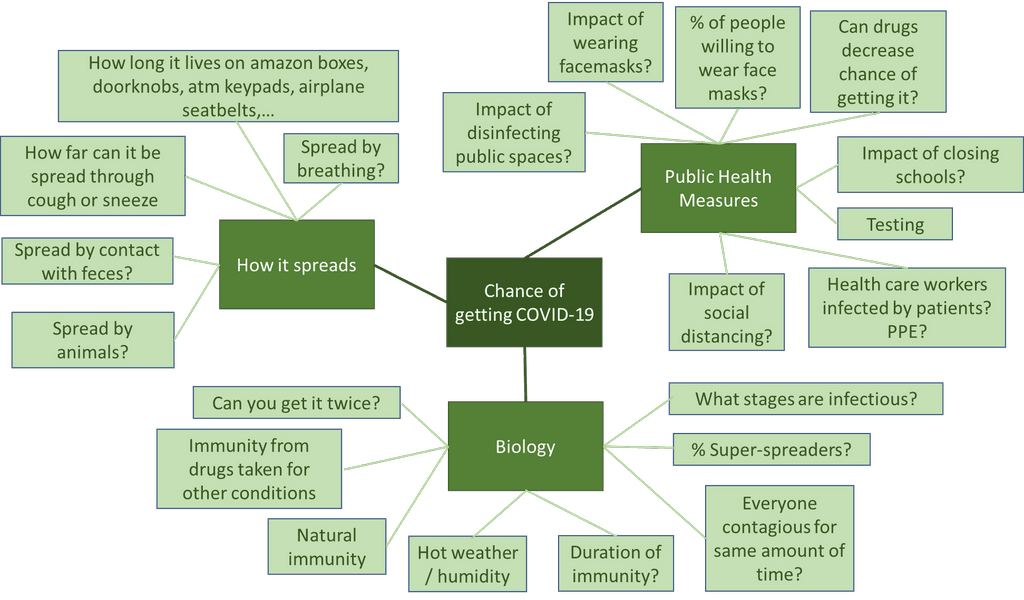
Notice that our understanding of several of these has changes over the course of the outbreak so far. Some will be removed, and some will be added as our understanding grows. Whether an infected person will die is equally complicated:
Messing up any of these effects will make a big difference when the population at risk is 350 million people.
For my next trick, I will estimate the risk of generalized anxiety disorder among epidemiologists.
Day 17
Another non-science thing I don’t want to forget. Today was my birthday. My parents called to wish me a happy birthday. My mother and father in-law called to sing happy birthday. My sister and her husband called to sing happy birthday. My brother and his wife and my 5 year old nephew sang to me over FaceTime and my sister in law even made a cake with candles (no flour, though, the shops are all out). My nephew blew out the candles for me. Too bad I couldn’t be with them and eat some. Other than that, I spent the day sewing face masks. We ordered Chinese food and it was nice not to have to cook.
Of all my birthdays, this is one where I’m so much more grateful to be alive than worried about more grey hair. And I have never had 3 sets of people sing happy birthday to me. But somehow it all left me so sad. I try to work really hard and focus on technical things to keep from the bitter morass of self pity. But I sure miss my family.
It’s Lent, which is a time when Catholics do their best to practice spiritual self-discipline. The pandemic is making all of us practice spiritual self-discipline. Usually this involves fasting - giving up food - to remind us that we can subjugate impulses to values. Now instead of food, we are denying ourselves freedom and human contact in service to a collective goal (say it with me - “bend the curve”). A traditional, spiritual fast is supposed to leave us humble, clear, wise, and open to transcending our current condition. I wonder what awaits us at the end of this secular and mandatory Lent (which is likely to extend well past Easter). Something good, I hope.
Of all my birthdays, this is one where I’m so much more grateful to be alive than worried about more grey hair. And I have never had 3 sets of people sing happy birthday to me. But somehow it all left me so sad. I try to work really hard and focus on technical things to keep from the bitter morass of self pity. But I sure miss my family.
It’s Lent, which is a time when Catholics do their best to practice spiritual self-discipline. The pandemic is making all of us practice spiritual self-discipline. Usually this involves fasting - giving up food - to remind us that we can subjugate impulses to values. Now instead of food, we are denying ourselves freedom and human contact in service to a collective goal (say it with me - “bend the curve”). A traditional, spiritual fast is supposed to leave us humble, clear, wise, and open to transcending our current condition. I wonder what awaits us at the end of this secular and mandatory Lent (which is likely to extend well past Easter). Something good, I hope.
Day 16
Most interesting question today: Is there any hope?
My thoughts:
Sure. Always. We really need a vaccine, but until we have that, we really need 2 things to get this under control. First, we need a prophylaxis that could protect our medical workers and maybe the highest risk patients. Second, we need a drug that can get moderate cases requiring hospitalization out of the hospital faster, or hopefully prevent hospitalization in the first place.
The prophylaxis need has some candidates, including chloroquine. There is a trial with a cool desigives chloroquine to close contacts of COVID-19 patients and will look at whether it can help reduce the rate of transmission to the contacts. This design should get an answer quickly. There is also a placebo-constudy of a tuberculosis vaccine which is underway in 1,000 healthcare workers.
And I’m happy to report an abstract for a clinical trial that might have some street cred in addressing the second problem. This study randomized 236 patients hospitalized with COVID-19 to Arbidol or Favipiravir (the Russian and Japanese versions of Tamiflu) and looked at the primary outcome of 7-day recovery. They found a 56% success rate in the arbidol group and a 71% success rate in the favipiravir group for patients with moderate COVID-19 requiring hospitalization.
Even among the real sickies with comorbidities, time to resolving fever and cough was better with favipiravir. There was no placebo group, and the efficacy of either of these drugs versus placebo for COVID-19 hasn’t been established. However, even arbidol could get more than half of the moderate cases requiring hospitalization discharged within 7 days, and favipiravir could get nearly 3 out of 4 out of the hospital quickly. This would free up medical resources for other patients. I’m sure I will find plenty to complain about when I see the whole paper, but this looks promising and is far better science than some of the other things we have seen so far.
So yes, finally, I have some reasons to be hopeful.
Day 14
Most interesting question someone asked me today:
Do masks work?
When the history of coronavirus is written, one of the great mistakes will be advising the public that we mortals (meaning non-medical folk) are incapable of operating a facemask. Most of us are able to do incredibly dangerous and complicated things including driving a car and shaving. Probably 8 out of 10 of us can manage slicing a tomato without a trip to A&E. How on earth do they expect us to wash our hands, which has about 15 steps, when we idiots in the general public can’t be trusted to use a facemask?
But this is the one that gets me (which our surgeon general has repeated):

Somebody please explain to me how incorrect use of a facemask can actually “be a source of infection”? I suppose if you lick the outside of the mask once you have worn it to a crowded place, that would be incorrect use that might be a “source of infection”. If this sounds like something you might do, please don’t try driving, shaving or slicing a tomato.
Countries that have gotten this thing under control like South Korea are advising people to wear masks when out and about. SARS-COV2 is so contagious that a 60 person choir an hour north of here held a practice with social distancing + hand sanitizer, but 45 are now sick with it and 2 have died .
Obviously, none but the best masks could protect us from a virus that can be spread by just breathing, let alone singing. But anything that could reduce transmission, even a little bit, could help our cause. And large droplets propelled by coughing and sneezing, which can travel > 6 meters, can also be stopped fairly easily with a mask made from an old t-shirt. It’s worth a shot.
Others have covered this topic in masterful detail, so I will direct to their work instead of trying to summarize it. There is a recent paper in Lancet with all the medical references for the efficacy of general mask use. If you have any questions about the physics of aerosolized virus-containing particles, let me recommend this piece. The pictures are spectacular. Or if you want to get into the weeds of the arguments for and against mask use, I recommend this review.
The history books will probably say that masks were not recommended to the general public because we couldn’t even keep people from stockpiling toilet paper, and there was no way that any masks would be available for our medical personnel if we encouraged the public to use them. Fine, all of that is probably true, and DIY masks are the answer to this one. But lying to us and saying they would not be effective just sews mistrust, which we really can’t afford.
Also, I think there would be at least a 20% reduction in transmission to health-care workers if we went back to old-school PPE:
[A picture containing text, book Description automatically generated]
Picture By I. Columbina, ad vivum delineavit. Paulus Fürst Excud〈i〉t. - Internet Archive’s copy of Eugen Holländer,Die Karikatur und Satire in der Medizin: Medico-Kunsthistorische Studie von Professor Dr. Eugen Holländer, 2nd edn (Stuttgart:Ferdinand Enke, 1921), fig. 79 (p. 171)., Public Domain, Wikipedia
Day 13
This is a question I’m writing about because I’m interested in it:
Why are the number of deaths increasing at apparently different rates in different places?
Hopefully the answer is public health policy and everything that follows is bullshit.
I found a cool new website where it’s possible to trace the coronavirus’s genomic evolution: NextStrain . People are sending in samples from all over the world, so a comparison of the sequences can be used to track the spread.
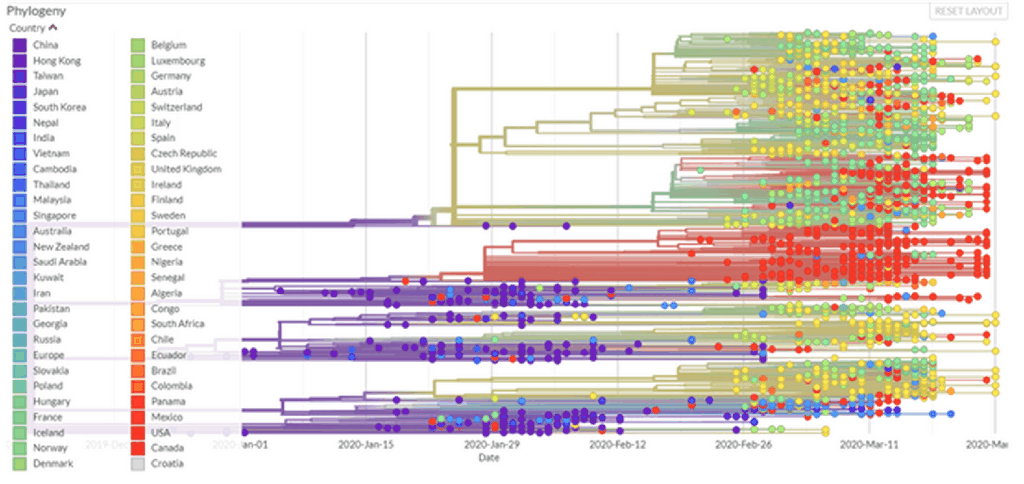
I find the radial view very helpful, especially when the data are filtered by country or city. Here are a couple examples that are on my mind:
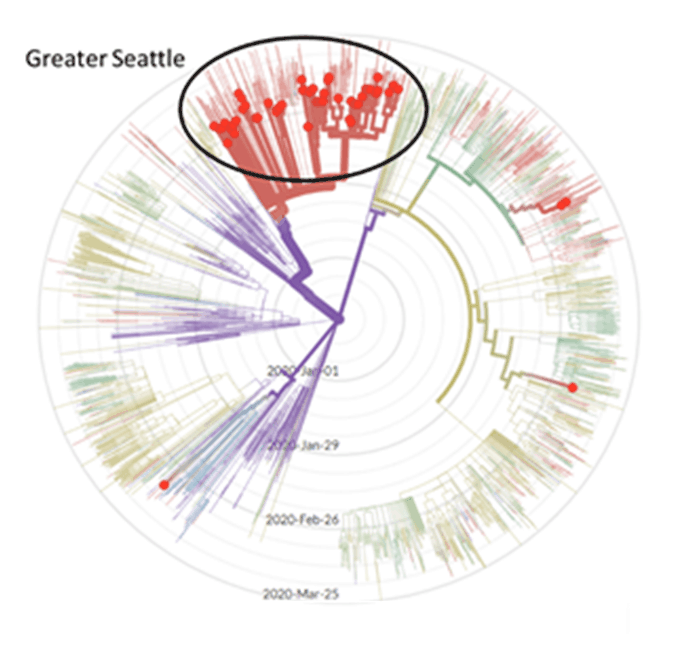
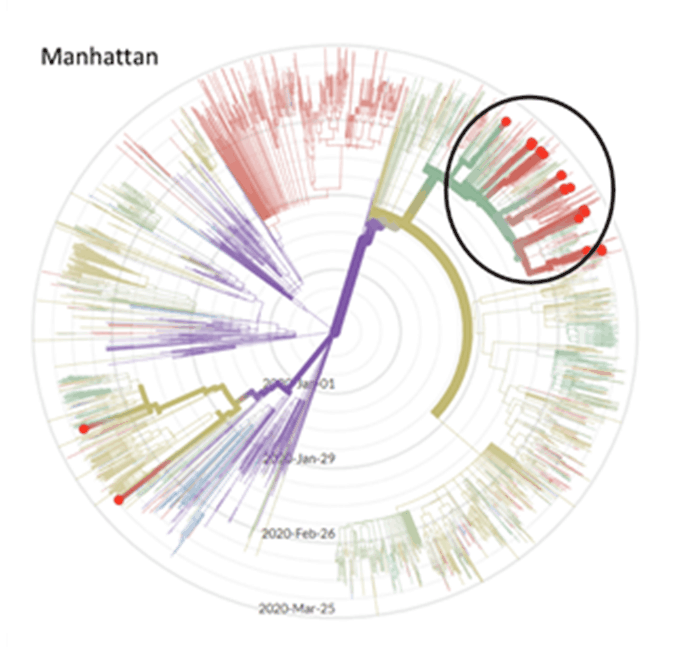
I know that in Seattle, our first case came from Wuhan on January 21. A researcher at University of Washington found a case of community spread that was descended from our first case, but in early March . We were surprised to learn it had been circulating for 6 weeks, and we really only noticed because it wrecked havoc on a nursing home resulting in a lot of deaths . On the East Coast, a case acquired through community spread is thought to be “patient zero” .
We are doing our best to socially distance here in Seattle, but I was shocked to see that our hospitalizations are down 20% , especially since our governor was concerned enough about our compliance to increase the restrictions on movement last week. We are being held up as an example of the benefits of social distancing, but it may be that whatever is killing people in New York isn’t even here yet. It would go a long way to explaining this graph:
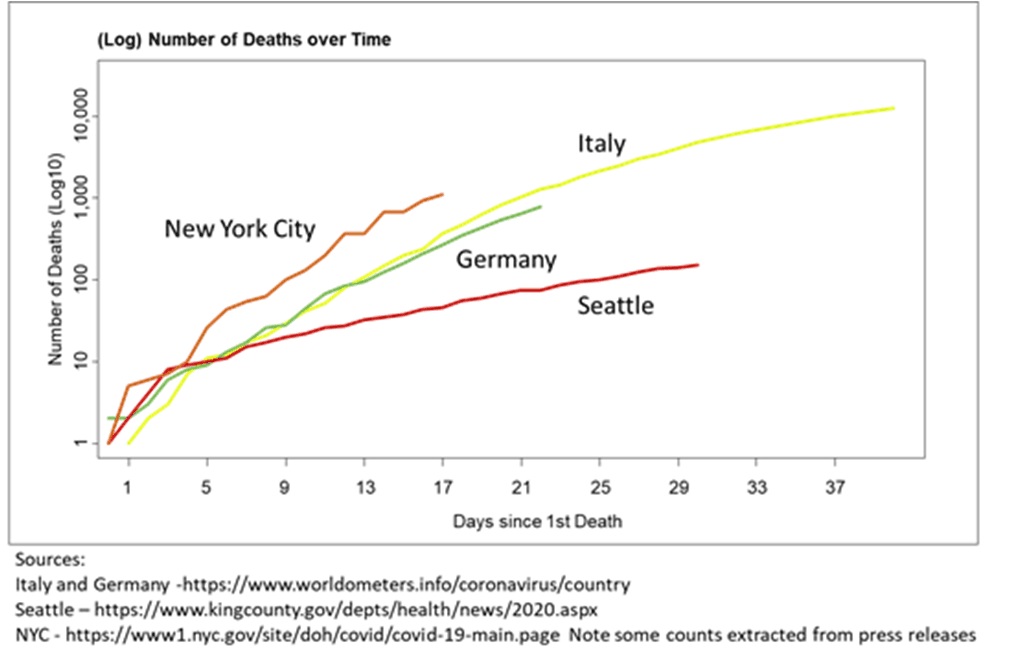
Please, God, if whatever is in New York is coming our way, let Corona-Lite have given us some immunity…
Day 12
Update to my Day 2 article:
There are some additional data out today about chloroquine and azithromycin:
This study reported on 80 patients “who received treatment with hydroxychloroquine and azithromycin for at least three days and who were followed-up for at least six days”. Same group as my concerns from Day 2. I sure wish I knew how many COVID-19 patients were treated at this hospital during the study period from March 3 to March 21. I went to the webpage of l'IHU Méditerranée Infection and found this:
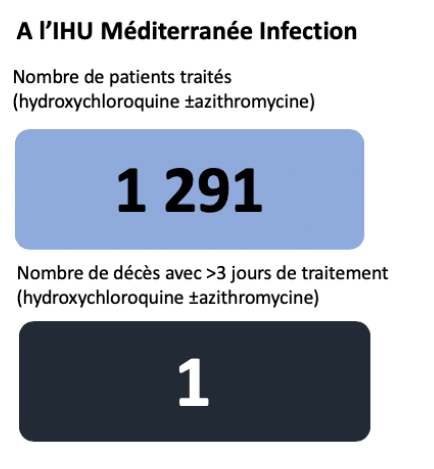
Which suggests that of the 1291 patients who received treatment with hydroxychloroquine for more than 3 days (with or without azithromycin), 1 has died. But it would be useful to know how many did not receive > 3 days of treatment, why, and what happened to them. The best evidence I have that this might work is that I haven’t seen any pictures of overwhelmed ICUs in Marseille on the news. These days…that’s not nothing.
I have seen only 1 30-patient randomized study out of China so far that shows no difference between standard care + hydroxychloroquine and standard care alone . The authors of the Chinese study note that “On day 7, COVID-19 nucleic acid of throat swabs was negative in 13 (86.7%) cases in the HCQ group and 14 (93.3%) cases in the control group (P>0.05)”. With n=30, this study has very little power considering that nearly everyone was negative by day 7, and so it is of little use as stand-alone evidence.
However, it is interesting that the new data from Marseille claim success because “A rapid fall of nasopharyngeal viral load tested by qPCR was noted, with 83% negative at Day 7, and 93% at Day 8” – pretty much the same rates as both arms of the small trial from China. Maybe most people just test negative after 7 days. It’s also interesting that only 15% of these patients had a fever.
There are larger studies in China and Italy which I have not seen yet that should provide better evidence of whether chloroquine is effective in treating COVID-19, and if so, which parameters it impacts.
I will keep you posted if i hear more on this treatment.
Day 11
Sorry folks some days i just have to rest!
Day 10
Day 10
28 March 2020
Most interesting question someone asked me today?
What is going on with the coronavirus testing?
Why is this taking so long?
When a coronavirus infects a healthy cell, the immune system doesn’t exactly know what has happened, but it sends out cells that find and destroy infected cells. This is the immune system version of “did you try turning it off and on again?”.
The immune system doesn’t even have to know what the problem is – it just blasts anything that looks infected. Like the technical support equivalent, this actually works a surprising amount of the time. If the initial immune response doesn’t get rid of the virus, the immune system figures out exactly what is invading cells and makes specific antibodies to neutralize that virus.
It can take some time for the immune system to work out the right way to kill the virus the first time it is infected, but if the same virus tries to invade a second time, the immune system remembers the first bout and sends out the more powerful specific antibodies right away. Sleep is what makes all this work, so if you want your immune system to work as well as possible, make sure you are getting enough sleep. Here is a picture of this process:
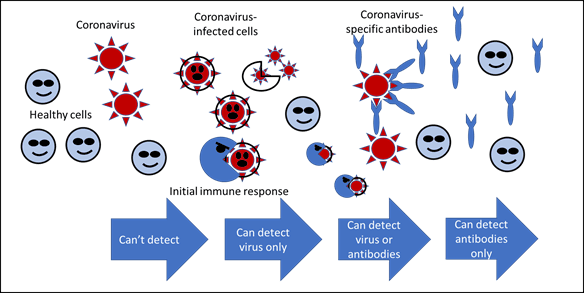
There are basically 2 kinds of coronavirus tests. Well, first let me clear up something I have been really sloppy about: SARS-CoV-2 is the name of the virus, COVID-19 is the name of the disease caused by the virus (like HIV and AIDS). The first kind looks for the SARS-CoV-2 virus (viral RNA) using a method called quantitative reverse-transcriptase-based PCR (RT-PCR). This is the test that the WHO recommended in January, and it requires capturing some live virus.
The virus attacks lungs, so in order to get cells that have been in lungs recently, an aggressive nasopharyngeal swab is needed. The CDC instructions are “Swab should reach depth equal to distance from nostrils to outer opening of the ear. Leave swab in place for several seconds to absorb secretions. Slowly remove swab while rotating it.”
When Donald Trump commented that there is “nothing pleasant” about this test, we know it was done correctly. A half-ass swab might not pick up any virus, which will result in a false negative and an infected person carrying on as usual and infecting others. False negatives are deadly in a pandemic, and this is probably why a home swab test was abandoned: if you had enough to drink to perform this test correctly, you might injure yourself and need scarce hospital resources. I am really hoping that the supposed cases of “repeat” infection are a correct swab (positive) followed by a half-assed swab (false negative), followed by a correct swab (positive) when symptoms persist.
This test for the virus is apparently fairly accurate, but I haven’t seen much actual clinical data. Somewhat terrifying, FDA has approved a score of these tests for emergency use , and only a few of these evaluated the accuracy of the tests in real people. Many used “contrived” (read: fake) samples to verify that the test would be positive when SARS-CoV-2 was present and negative when SARS-CoV-2 was not detected.
Just 3 tests describe the positive predictive value, which is the chance that someone with a positive test actually has the disease. One of those was the CDC test, which failed completely. Since all of these are looking for viral RNA, either a lab or an expensive machine is required to process the test. A big hospital might be set up to do these tests, but a doctor’s surgery would not be.
So though there was a lot of excitement about 45 minute (Cephid) or even 15 minute (Abbott) results, these will realistically only be useful for people in the hospital. Spain bought a lot of rapid tests from China (not Cephid’s or Abbott’s), and found that they were only detecting SARS-CoV-2 30% of the time. A test involving flipping a coin and claiming the virus is present if it lands on “heads” would have a much lower false negative rate.
The other approach to testing is immunoassay, which means looking for antibodies as we do in HIV screening tests. This kind of testing might not be able to detect the virus until the immune system has fought it off. Knowing somebody had the virus would not help while the patient is sick, but would identify them as someone with possible immunity now. An immune person could work on the front lines of this crisis with lower risk, or the antibodies in their blood might help the virus in someone who is currently sick.
Theoretically these tests could be administered at home with a drop of blood and give rapid results, but the accuracy is unknown. One of the promising new ones in US out of Mount Sinai Hospital correctly identified the virus in a small study of 4 patients, New blood tests-true scale coronavirus pandemic?, which is a good start but further testing is needed before we bet the farm on this test. UK has purchased 3.5 million antibody tests, but I have not yet seen information about their accuracy and it appears these data are currently being collected.
Both kinds of tests are needed, but they need to be administered at the “right time” in the disease, and we don’t even know exactly what that means. If a test for the virus is given too early or too late, or the swab is not aggressive enough, it will produce a false negative. If an antibody test is given too soon, it will not detect immunity.
I took care of my 83-year-old mother who had a persistent fever and fatigue for a week, and finally pneumonia. Since she didn’t need to be hospitalized, she was not considered high enough risk to be tested. I’m happy to report that she is well on the way to mended, but last week I had a low-grade fever and fatigue (and a bunch of other symptoms that were probably psychosomatic). I believe that I had whatever she had, but I don’t know if it was COVID-19. I hope so, and that we are both immune now, but I see the danger to myself and others in acting as if I am immune when I don’t know for sure.
Here is a more technical article about the state of SARS-CoV-2 tests.
Day 9
27 March 2020
Most interesting question someone asked me today:
Have you finally got the outbreak under control in Seattle?
My thoughts on this (continued): I used the King County Department of Health andNew York City Department of Health web sites to get the most recent distributions of age and gender for cases and deaths.
They are:
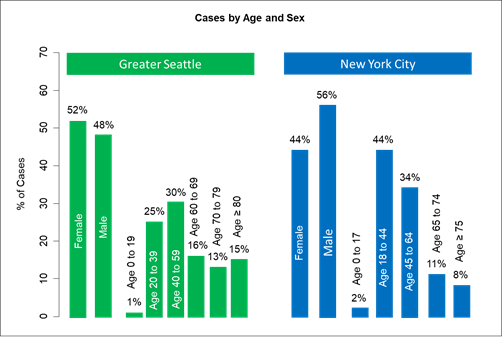
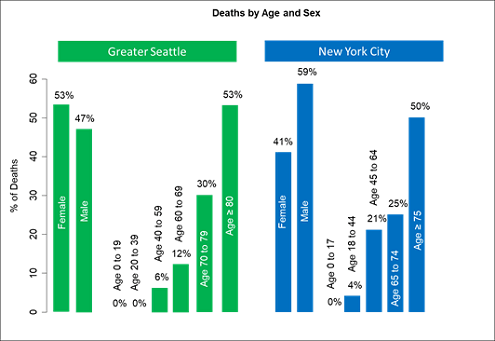
Couple of observations. Compared to Seattle, New York has more cases who are young people (< 40). In Seattle the young people who are being tested are first responders – testing has not expanded much beyond that for young people. The percentage of male cases is higher than for women in New York; the distribution is closer to even in Seattle. In New York, 4% of deaths are in patients age 18 to 44.
Fortunately, we don’t have any deaths in patients < 40 (yet). Most interesting, there is actually a statistically significant difference in the gender distribution of deaths. Compared to Seattle, a higher proportion of men are dying in New York City (47% vs. 59%). I have described that Seattle has a similar proportion of smokers of both genders, while 17% of men and 9% of women in New York smoke [https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief103.pdf]. This is a smaller gender difference than in China and Italy, but larger than in Seattle, where 14.7% of women and 17.9% of men smoke.
[https://www.doh.wa.gov/Portals/1/Documents/Pubs/340-240-TobaccoRelatedDisparities.pdf]. So the gender death distribution in New York is more like in China and Italy, while Seattle may be different. One difference could be that men are more likely to work outside, and the air quality in New York is not always great compared to Seattle. The extra x chromosome in women should confer additional immunity, but why that would be different in Seattle compared to New York is unclear.
Though the risk of seeing this difference by chance alone is only 1/50 (p=0.02), it is still early and may change. I will look at San Francisco and Los Angeles to determine if they are more like Seattle or more like New York.
Day 8
26 March 2020
Most interesting question someone asked me today:
Most interesting question someone asked me today:
Have you finally got the outbreak under control in Seattle?
My thoughts on this: Hell no. It’s going to take a couple posts to describe some of the differences between King County (greater Seattle area) and New York City. We had our first case before NYC, and our first case was actually our first death reported 3 days after that person died. We had 39 deaths by the time NYC had 1 death.
As it stands now, NYC is testing about twice the proportion of the population we are (0.55% in Seattle and 1.0% in NYC). They are also testing a different set of people; about 26% of their people tested are positive compared to 12.8% of our tests. We are testing first responders (nearly all negative), hospitalized people with respiratory problems (nearly all positive), and very high-risk symptomatic people (mixed, I am trying to get more specificity on each of these groups).
I won’t comment on the very important distinction between the public health slogans. I will note that NYC has 28,146 people per square mile compared to 968 for us. In terms of the spread of a highly contagious disease, that makes a big difference. Coming tomorrow: a comparison of who is testing positive and who is dying.
Day 7
Today I have a story, not an analysis.
My friend cut the hell out of her hand making dinner. She is in her 70s, and her daughter called the local A&E to ask if my friend should be brought in to have it stitched. The doctors on shift said that yes, they should stitch it, but the waiting room was full of people with flu-like symptoms, and the risk to my friend of catching coronavirus was higher than the risk posed by the cut.
My friend cut the hell out of her hand making dinner. She is in her 70s, and her daughter called the local A&E to ask if my friend should be brought in to have it stitched. The doctors on shift said that yes, they should stitch it, but the waiting room was full of people with flu-like symptoms, and the risk to my friend of catching coronavirus was higher than the risk posed by the cut.
The doctors supervised over Skype as they talked my friend’s daughter through how to stop the bleeding and bandage the cut, and planned a daily video conference to inspect how it is healing and to check for infection.
I have been worried that overwhelmed medical systems would be unable to treat the day to day accidents and injuries we all experience, but I hadn’t thought about doctors needing to weigh the risk of exposing a patient to a contaminated hospital against the risk of DIY laceration treatment.
I have been worried that overwhelmed medical systems would be unable to treat the day to day accidents and injuries we all experience, but I hadn’t thought about doctors needing to weigh the risk of exposing a patient to a contaminated hospital against the risk of DIY laceration treatment.
I need to update my predictions about excess morbidity and mortality - disease or death that could usually be prevented. These outcomes are collateral damage in the war against COVID-19, but they need to be counted to quantify the misery of this situation. Mostly, when things go back to normal, I want to remember that decisions like this had to be made.
Day 6
Most interesting question someone asked me today:
Does social distancing actually help prevent disease spread?
My thoughts on this: I think so. The simplest summary measure of the “contagiousness” of a disease is called R0 (pronounced “R-naught”). Basically, R0 is the number of new people that each infected person can spread the disease to. It has 3 components:
The horrible “Spanish” flu of 1918 (which may have started in the US) had R0 around 2, so each infected person was on average infecting 2 new people. The typical flu has an R0 around 1.3, so if 3 people get the flu, 2 of them will infect 1 new person and 1 of them will infect 2 new people (on average). The R0 of measles has a lot of variability and should be calculated for a specific place and time, but it is frequently estimated to be between 12 and 18. Last year there was a measles outbreak at Disneyland , and because it is so contagious and Disneyland is so popular, this was terrifying for everybody who follows infectious diseases. Based on the typically cited range, a single person with measles will infect 12 to 18 new people. Yikes!
Luckily, R0 isn’t entirely a property of the disease. Everything we are throwing at COVID-19 is to try to make that number as small as possible. The first part, transmissibility, is a property of the virus. The mode of transmission (basically airborne or spread through bodily fluids) is usually a fixed thing specific to the disease.
All we can do to minimize the first term is to try to stand 6 feet apart and wash our hands like our lives depend on it. The second term, contact rate, we can do slightly more about. Ideally, we can reduce the contact rate with a vaccine. A vaccine is biologically like being infected. So if a high proportion of a population is vaccinated, the chance of an infected person having contact with an unvaccinated person is really low.
Until we have a vaccine, we have to reduce the chance of an infected person running into an un-infected person by simply reducing the amount of people an infected person can have contact with, which is what social distancing is meant to do. Finally, the study about azithromycin and hydroxychloroquine that I was complaining about the other day did one thing right, which I didn’t mention then but will now: they measured whether the drugs shortened the number of days that infected people are contagious. Hopefully this drug combination, or some drug combination, can do this. It would help to slow down this pandemic, along with helping our infected medical workers recover sooner.
Part of why we underestimated COVID-19 is that we didn’t know at first that people can spread it before they have symptoms, so the number we stuck into the formula for how long people are contagious was way too low.
My husband just pointed me to a really neat app – and excellent use of data – that usescell phone location to track how we are doing on social distancing: .
Here is the graph for Washington State – March 13th was the day the schools were closed and everyone rushed out to pick up beer and loo rolls, expecting some kind of quarantine. Our governor, who is much better at marketing than pretty much anything else, finally gave the order yesterday that we should “Stay Home, Stay Healthy”. It even has theme music. He thought “Shelter in Place” sounded too scary. As you can see from the graph, we were going the right direction with social distancing anyway. There are still some selfish people not taking this seriously, and the other thing that happened Monday was the national guard arrived. I hope this is not to enforce social distancing, I hope it won’t be necessary. I also hope someone is working on something similar in UK.
Day 5
Most interesting question someone asked me today:
Who will suffer most if NHS is slammed with coronavirus patients?
The answer to this one surprised me: Looking at the Hospital Episode Statistics dataset, the average monthly number of A&E attendances across NHS last year was 1,812,000 (among patients with recorded age). And 502,047 of these A&E attendances every month are for people ages 20-39. So what will happen if there are half a million patients every month who need emergency care but can’t get it because the entire NHS is treating COVID-19 patients?
In US during the 1918 influenza, people knew the hospitals were completely overwhelmed and started kidnapping nurses (Barry JM. "The Great Influenza: The Story of the Deadliest Pandemic in History”. London: Penguin Books; 2005, pg 277). If you need an emergency appendectomy, the logistics of kidnapping the staff required will be rather complicated.
The elevated rates of A&E attendances in younger adults has been reported by others, who blame this increase on “poor understanding regarding appropriate use of ED services, a lack of knowledge of other health services available, and poor access to primary care”. Personally, I spent my 20s figuring out what I didn’t want my life to look like, and this included a few attendances at A&E. But if you are young and need yet another reason to comply with social distancing and not contribute to worsening the problem for NHS, do it out of self-interest – statistically speaking, there is a good chance you might need their help.
Day 4:
Most interesting question someone asked me today:
Are 40% of the people hospitalized for COVID-19 young?
My thoughts on this: I think Dr. Deborah Birx, who I admire very much, was trying to persuade teens that they need to take social distancing seriously. Based on the CDCs own report , the distribution of age in US hospitalized patients through March 16th looks like this:
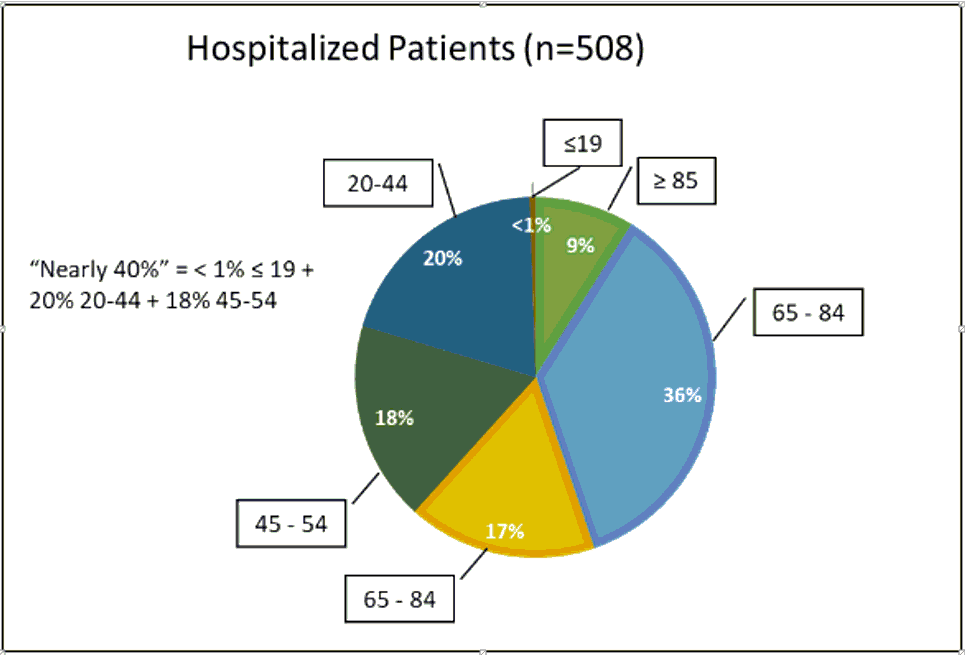
So 20% of hospitalizations in people 20-44 + 18% of hospitalizations in people 45-54 + a couple people ≤19 is about 38%, which is “nearly 40%”. There is a great book called “How to lie with statistics” by Darrell Huff which I would recommend to anyone, but this is the trick of combining categories that aren’t the same to make a point.
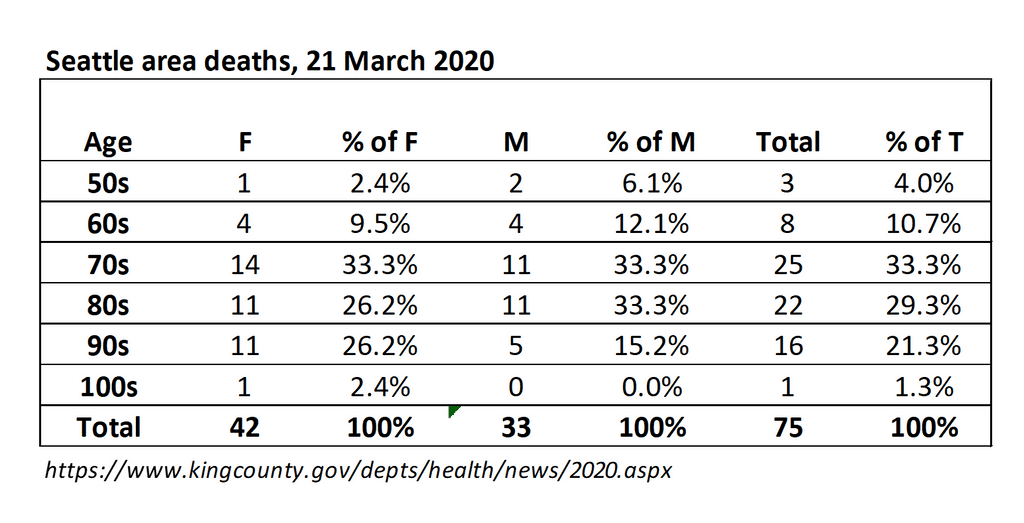
Looking at deaths, nearly all of the early ones were in the Seattle data, so my data are more granular than in the CDC report because of good initial reporting from King County Public Health.
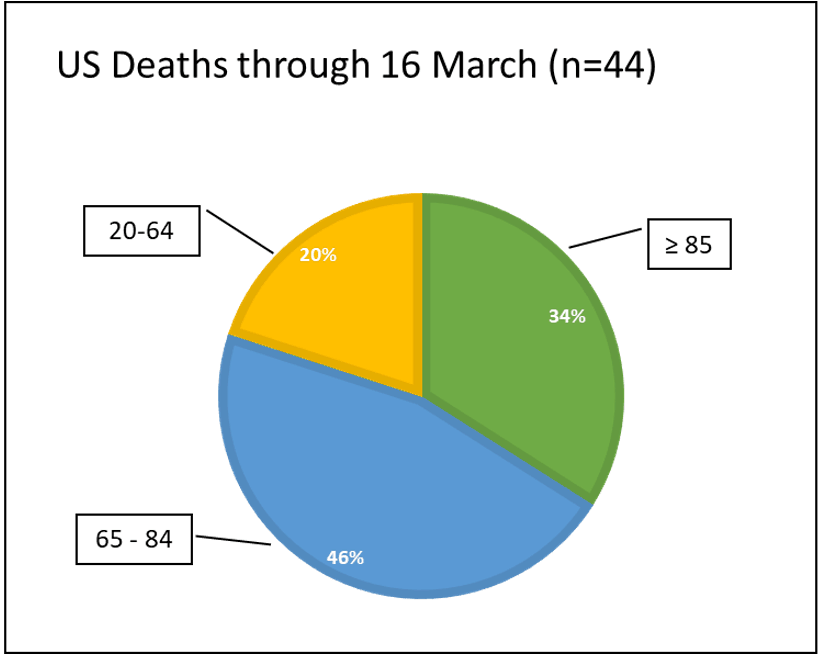
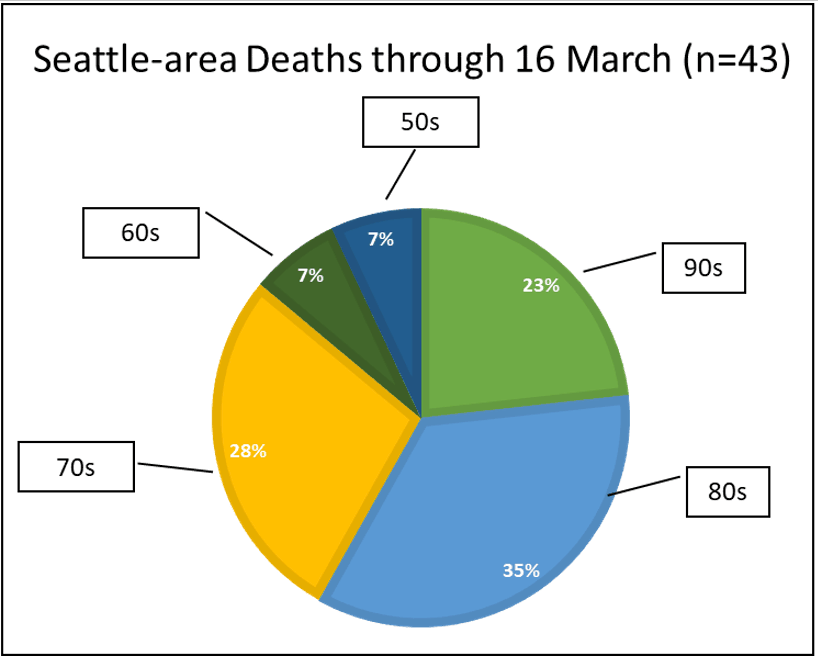
In this case, the CDC is combining ages 20-64, which is an enormous range. King county has the data by decade, and there were no deaths in anyone under 50. The 20-64 range I find a bit misleading.
The way I would have made Dr. Birx’s point is with the distribution of age among hospitalized patients through March 4th, when King County stopped publishing details of individual cases:
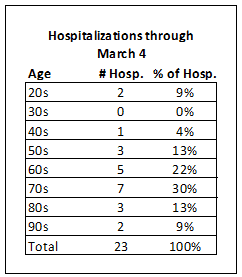
So 9% of hospitalized patients, or almost 1 in 10 using the rounding convention above, were in their 20s. And since these 20 year olds are at the hospital up the street from me, I know that the last report said that they were in critical condition in ICU. So if you are a young person, please, please hang out in your room and play video games instead of sneaking out to see your friends.
Day 3
Most interesting question someone asked me today:
Why are men at higher risk of dying from coronavirus?
My thoughts on this: There are some concerning data from the 2 most heavily infected countries, China and Italy, that suggest men are more likely to die from coronavirus than women. The data from Seattle don’t show a significant difference (I get a difference < 1% in the crude rates), but that may change:
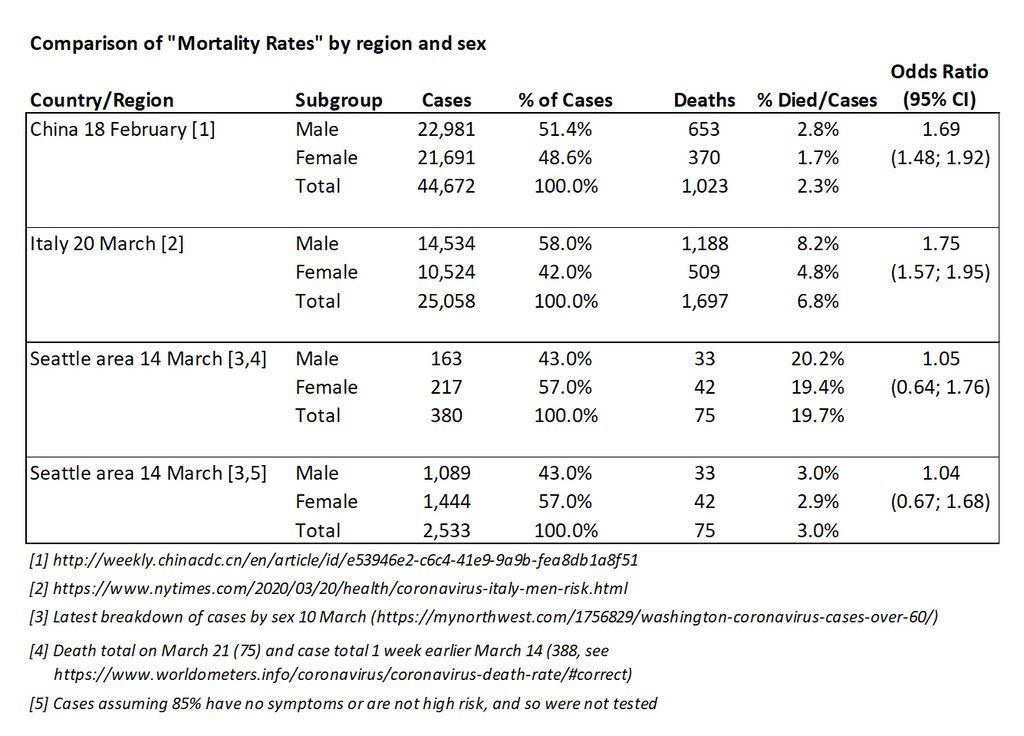
So based on the data I have, it doesn’t appear than men in the Seattle area are more likely to die than women. There are many issues with calculating death rates while an outbreak is ongoing, and biases due to who we are currently testing, so these factors could change my answer. A gender shift in who we are testing since March 10th could also change things. In Seattle, a higher percentage of cases were female, which is also different than China and Italy. The differences in China and Italy have been blamed on differences in smoking rates.
48% of men and 2% of women smoke
30% of men and 19% of women smoke
Since COVID-19 infects lungs, and this seems to be why people die from it, the smoking differences may explain the mortality differences. The gender gap in smoking
In Washington state 14.7% of women and 17.9% of men smoke
There also appears to be some protection from the extra X chromosome, which would genetically be an advantage for women. die of SARS compared to women , but this finding may suffer from similar differences in smoking. I will keep an eye on the gender difference in death rates, but I don’t see any evidence of it in the Seattle data so far.
If anyone is curious, our current deaths by age and sex are as follows:
Day 2
Most interesting question someone asked me today:
Will gin and tonic cure coronavirus?
My thoughts on this:Tonic water (first used to treat malaria) contains a very small amount of quinine, which is related to chloroquine. Donald Trump has extremely high hopes for it while our top infectious disease doc Anthony Fauci is not convinced that it will get rid of coronavirus. The Chinese studies are not out French study Chloroquine might work. It worked for the original SARS 20primate tissue study.
This new study…sounds like it was conducted in the middle of a terrifying pandemic. The plan was to have 48 patients and try to shorten the duration of illness, but they ended up with 26 hydroxychloroquine and 16 control subjects. The patients were not randomized to control or hydroxychloroquine; all the kids and the patients who didn’t want or couldn’t take hydroxychloroquine were the control patients. This design is not great for an experiment because you start off with 2 groups that are not the same, and then if the outcomes are different, you can’t tell if this difference is due to the drug. In this case, 4 of the control patients are kids ages 10, 10, 12 and 14, while the youngest patient in the hydroxychloroquine group is 20.
Of the 26 hydroxychloroquine patients, 6 patients were thrown out of the analysis: 1 left, and the 5 others had something bad happen (deathx1, transfer to ICUx3, nausea causing discontinuationx1). With the bad outcomes thrown out of the hydroxychloroquine group, the results look good: 14/20 or 70% of hydroxychloroquine patients were virologicaly cured compared to 2/16 or 12.5% in the control group. This is somewhat misleading. Five of the control patients didn’t have the test on day 6, and they are assumed to be failures.
One patient in the hydroxychloroquine group didn’t have a test on day 6, and was assumed to be a success. When the 5 patients with known bad outcomes are put back in as failures, and the same assumption for missing data is made in both arms, the numbers are 58% versus 12.5% if we treat all missing as failures, 50% versus 44% if we treat all missing as successes. The missing data matter a lot! There were also 6 patients in the hydroxychloroquine group who were given azithromycin “depending on their clinical presentation” (chlamydia, anthrax…bacterial pneumonia?). Whoever these 6 patients were, they did extremely well, which further helped the hydroxychloroquine group.
This study isn’t evidence that hydroxychloroquine will be a wonder drug. It might persuade me to do a bigger, better study. A lot of people are taking chloroquine in the hope that it will prevent COVID-19 infection. I don’t see any evidence of that (#TeamFauci), but this may be the year we get rid of malaria. To summarize, I wouldn’t count on gin and tonic to save you from COVID-19. I could probably do a study this afternoon to demonstrate that gin and tonic will hinder one thing that does work: social distancing. Any volunteers?
20th March 2020 - Day 1
Most interesting question someone asked me today:
Are you worried about having packages and things delivered?
My thoughts on this: We are learning more about how long COVID-19 can live iNEJM article. I brought some frozen meat and non-perishable groceries to some friends hit especially hard by the economic changes over the last few weeks. This family has 2 adults who usually work full time, but they both do custodial work at a hotel and their hours have been cut down to 8 per week, so right now there is no money for anything.
I delivered a bag to their doorstep and instructed them not to open the door when I arrived. I suggested they use disposable gloves to take everything out of the bag and disinfect it with bleach and water (4 teaspoonCDC Cleaning/Disinfection). I suggested they let everything air dry before bringing it into the house.
Amazon has been a godsend for those of us who can afford it (more on the emerging delivery class divide later), and they are hiring 100,000 additional employees to keep up with demand. But what about those boxes? Are they contaminated? I have no idea. The paper above suggests that COVID-19 can live on cardboard for up to 48 hours.
One friend is leaving the boxes outside for 2 days. She has bears in her neighborhood (yes, we have bears 30 minutes from downtown Seattle), so I’m not sure how long that will last if she is ordering anything they fancy. Also, this is not a good strategy with anything perishable as our health resources are needed for more important things than preventable foodborne illness. I am disinfecting the outside of things and wherever possible removing outer packaging.
There is a terrific Invisible hands, who are shopping for seniors . This is a brilliant idea because it gives young people something to do besides clutter up Florida beaches, and prevents vulnerable people from having to go to the grocery store. But as these efforts increase, there will be more questions about receiving packages and potential contamination. I’m fairly sure the risk is much lower receiving deliveries and giving things a wipe-down or wash compared to physically going to the grocery store, but will update as evidence-based guidelines (or at least eminence-base guidelines) become available.
Help researchers help you!
Take part in this novel research to make a change
- Share your opinion as your voice matters
- Help us understand everyone’s experience
- No bias, just science
- Help us improve future responses
AMO sends your votes securely via standard SMS, these are usually included free in UK airtime bundles. Ask your mobile supplier if you get inclusive SMS to standard UK mobiles.